The nation’s healthcare delivery system appears to be in constant political flux. While much remains uncertain, one thing remains true: there is bipartisan support to move the healthcare system away from the traditional fee-for-service model. This means that—no matter what occurs in Washington—hospitals will continue to transition to value-based care through reimbursement models and payment penalties that reward the value of care over the number of visits and tests ordered.
I recently attended a conference session on value-based purchasing strategies that I found eye-opening. While the approaches shared by the administrative hospital leads were impressive, that was not what captured my attention. What did capture my attention was the audience. Most of the seats were filled by supply chain professionals despite the fact that the actual content of the session did not speak to their role. Supply chain’s part in value-based care is not often seen or heard at a high level despite being vital to a provider’s ability to deliver quality care at a lower cost. In considering value-based purchasing strategies, we need to be careful that we aren’t leaving these important stakeholders out of the conversation.
A look back at the history of healthcare delivery reveals how the function of the supply chain has evolved alongside reimbursement policies—from unfettered purchasing when reimbursement was largely open-ended to a focus on cost containment as healthcare spending escalated. This era is no different. In fact, the supply chain has never been more important or in a better position to make a positive impact on healthcare and the lives of patients. Today’s supply chain must be strategic, expanding its focus beyond product cost to examine all healthcare delivery costs and their correlation to care quality and financial outcomes. It is called the intersection of cost, quality, and outcomes—also known as CQO—and the place every healthcare organization should be striving to reach.
Supplies—whether they be as simple as gauze or as complex as neurostimulators—are essential to patient care. Today, providers must be able to quantify and weigh a product purchase based on the impact of that decision on the clinical and financial outcomes of the procedure for which it is used. The supply chain sits at the center of these decisions, which is why supply chain professionals are particularly well suited to lead CQO initiatives. But while CQO provides the decision-making framework, hospital leaders must still find ways to ingrain these practices into and across their organizations.
This is no easy task, but it’s easier when you know where to start. The first step lies in readying the supply chain for value-based care, which can be viewed as a succession of several smaller objectives:
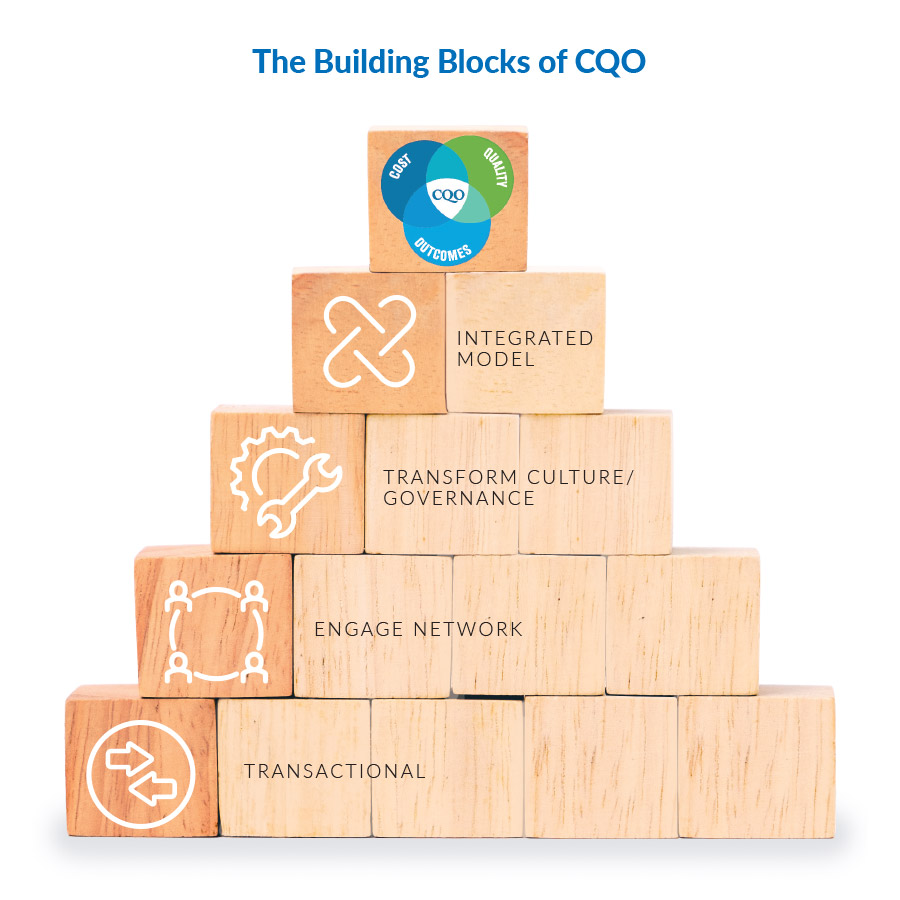
Transactional: A transactional supply chain is focused on price improvement and performing fundamental supply chain tasks.
Engage Network: On the path to operating at the intersection of CQO, the next step for supply chain is engaging a network of C-suite executives, suppliers, and product end users (e.g., physicians, clinicians, and service line leaders). To make evidence-based purchasing decisions most effectively, supply chain professionals must understand the needs of others and incorporate feedback into the sourcing process. This greater level of understanding helps move the provider-supplier conversation from one of price over value to healthcare issues over supply chain issues. It also cultivates a relationship that is more truly aligned with value-based care.
Transform Culture/Governance: Once the supply chain has the support of an expanded network, department leaders are better positioned to make the more significant cultural and structural adjustments that are needed to facilitate change as well as to begin examining, learning about, and familiarizing their teams with alternative data sets so they are armed to make better-informed, value-based purchasing decisions.
Integrated Model: An integrated model is achieved when purchasing goals are aligned organization-wide. At this stage, hospital administration, end users, and supply chain are employing data to focus on how products are used and the differences in quality based upon the total cost of an episode of care.
Cost, Quality & Outcomes: When all stakeholders are focused on securing results that decrease costs while improving quality and outcomes, the supply chain is operating at the intersection of CQO.
Today’s healthcare supply chain must evolve in line with the industry’s shift to value-based reimbursement, as the performance and effectiveness of the supply chain are integral to a provider’s ability to deliver high-quality, cost-effective care in a challenging economy. The ability to take a more strategic approach to product selection, looking for the best value (examining total cost, quality, and outcomes) rather than simply the lowest price, begins with the supply chain. Acurity’s member-centric model identifies where your supply chain is in the spectrum above and lays out a roadmap to get you to where you need to be.
Together, we will improve healthcare through the supply chain.

Comments are closed.